Safeguarding the Future of Not-for-Profit Healthcare
We are mission-focused, not profit-driven
Sutter’s mission and the purpose of not-for-profit health systems and hospitals is to do everything we can to ensure our patients and communities receive the care they need, when they need it.
We invest in community health programs, fill healthcare gaps and increase access to care. Our hospitals care for everyone, regardless of insurance or ability to pay, and we are an essential part of the communities we serve and the public health safety net they rely on – as demonstrated so acutely during the pandemic.
But mounting cost pressures and growing competition from for-profit interests put not-for-profit healthcare under pressure and potentially at risk if they remain unchecked.

We invest in patients and communities – that’s our priority
Not-for-profit health systems do not have shareholders or investors to answer to — instead, they invest revenues back into care delivery. Sustaining this model is vital to communities and patients.
We improve the quality of care
- $71.6M+ spent each year to research and develop new cures and treatments
- 100+ clinical trials launched every year
- Ranked within top 3 nationally in overall quality on Premier’s 15 Top Health Systems® for 2025 – the only California system to make the list
- 7 Sutter hospitals were named among Healthgrades’ America’s Best Hospitals, with four placing in the top 50 for overall clinical quality
- In 2024-2025, 5 Sutter hospitals were named among US News and World Report’s Best in California, 16 received “High Performing” recognitions in at least one quality measure, and 3 campuses were named in the Top 50 nationally for medical specialties


We make it easier to access care inside and outside the walls of our care facilities
- $4.6B in community benefit investments, including charity care, support for community health programs, and unreimbursed care for Medi-Cal patients over the past 5 years
- Nearly $50M invested over the past 5 years to support Federally Qualified Healthcare Clinics that provide free and affordable community care
- Opening 27+ new ambulatory care centers, 27 urgent care sites, and 22 ambulatory surgery centers over next few years
We train tomorrow’s healthcare workforce
- We are building capacity to train 575 residents and fellows at 39 accredited GME programs across our system by the end of 2027.
- Academic partnerships that support medical school students and accelerate nursing and allied healthcare training programs.
“Even as we shoulder the weight of a strained national healthcare system and mounting financial pressures, our commitment to patients remains unwavering. Their well-being is not just our mission—it is our measure of success.”
- Katie Nair, Sutter Health Administrator and Member of the California Board of Registered Nursing

The cost pressures and shifts we face
Not-for-profit health systems like Sutter Health are on the front lines of patient care every day. Because of our role, we face a number of cost pressures – many shifted to us by other segments of the industry that generate significant profits for the benefit of their shareholders and Wall Street.
According to the California Hospital Association, California’s Office of Health Care Affordability’s report on healthcare spending trends in the state from 2022-23, released June 5, 2025, found “the biggest drivers overall of increased health care costs were insurance companies and pharmaceutical companies.”
CHA offered these highlights from the report:
- In all, total health care expenditures in California grew by 8.2% (from $378 billion to $409 billion) from 2022 to 2023.
- Nearly 17% of that growth supported higher health insurance company profits, not patient care.
- In fact, insurance company administrative costs and profits ballooned more than 23% in 2023, while hospital spending grew less than 5% (inpatient hospital spending grew at an even lower rate, a mere 2.3%).
Drug prices
Rapidly growing Medicare population
Medicare paid just 83 cents on every dollar hospitals spent caring for patients in 2023— resulting in a shortfall of almost $100 billion nationally. This pressure mounts with 11,000 new patients aging into Medicare daily.
Inadequate government reimbursement
Nearly a quarter of the patients Sutter Health serves in our hospitals are insured by Medi-Cal. Because the State of California under-reimburses for this care, Sutter invested $665 million more than the state paid to care for patients with Medi-Cal in 2024. Medicare’s reimbursement also does not keep pace with the cost of care. According to the American Hospital Association, “from 2022 to 2024, general inflation rose by 14.1%, while Medicare net inpatient payment rates increased by only 5.1% — amounting to an effective payment cut over the past three years.” Recently federal legislation has introduced new uncertainty here.
Commercial health insurer payment delays and denials
Nationally, for-profit commercial health insurers generate billions more in revenue, while working to minimize how much they pay hospitals and physicians for medically necessary care. They also add onerous administrative requirements into contracts to make it easier for them to deny and delay that payment.
What’s at risk?
Increasing financial and market pressures can create instability for not-for-profit systems working to deliver comprehensive high-quality care, make investments to fill community health gaps, and improve access to care and well-being.
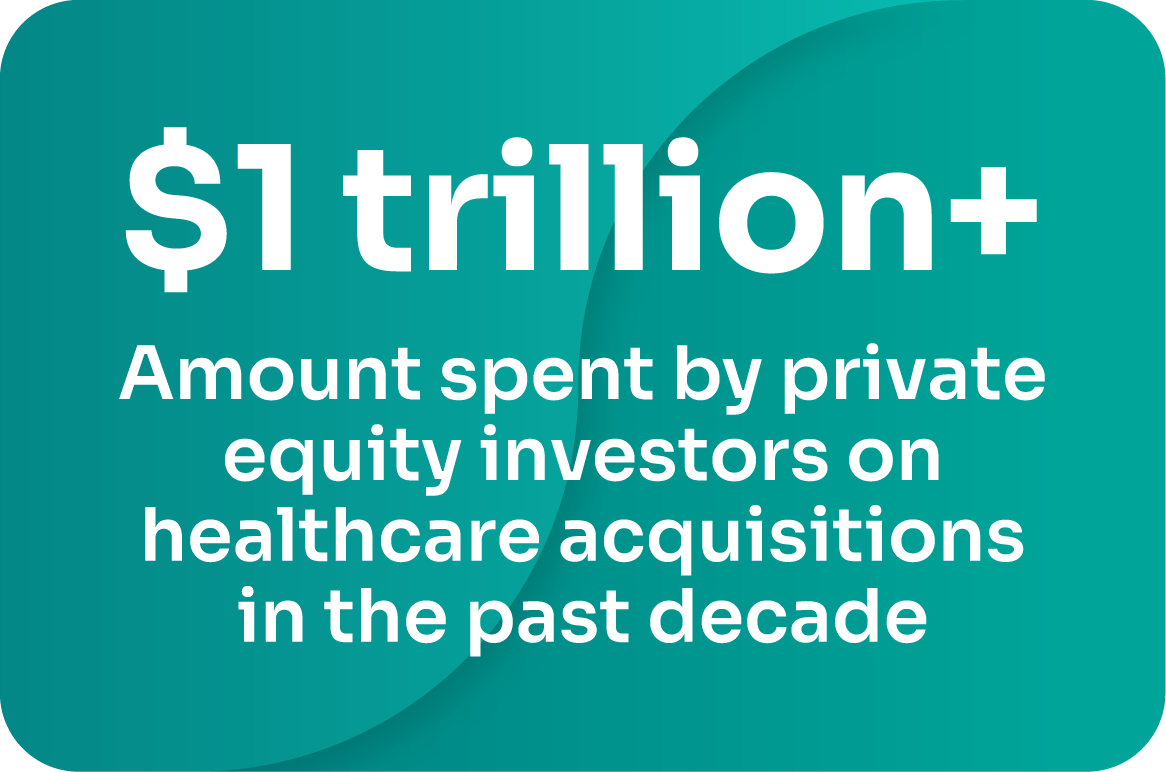
When not-for-profit health systems and hospitals falter, it’s most likely that for-profit, often private equity-funded, healthcare entities with very different missions – will step in to fill the void. Many are now entering the market as competitors to cherry pick the easiest and most cost-effective care to provide – all of which threatens to segment and fragment care, which is not in patients’ best interests.